Source [David Orenstein, Picower News | November 2, 2023]
Picower Institute-based collaboration will study mechanisms that might enable peripheral immune cells to deliver a potentially therapeutic molecule to the brain.
A new three-year research project, funded by the Simons Center for the Social Brain at MIT, posits that the immune system can be harnessed to help treat behavioral symptoms of autism.
In 2020, Associate Professors Gloria Choi of MIT and Jun Huh of Harvard Medical School showed that the immune system “cytokine” molecule IL-17a, when applied to a particular brain region in mice modeling autism, improved social behavior and reduced repetitive behaviors.
The study in Nature provided an explanation for reports by many pediatricians and parents that some people with autism improve in these ways when they happen to experience an infection. In mouse models, the team showed that peripheral immune cells, if they had been primed while in utero by a maternal infection, increased IL-17a when the mice sensed a new infection. In the brain, the molecule happens to calm the hyperactivity of neurons that produces the autism symptoms. The researchers also showed that even when other mouse models of autism did not have immune systems primed by maternal infection, their behavioral symptoms improved if IL-17a was directly injected into the brain.
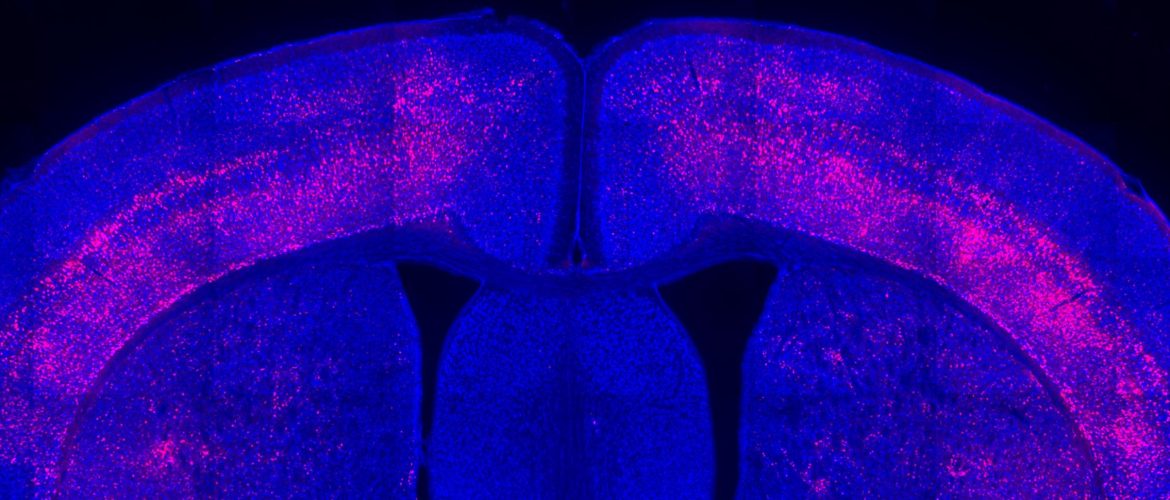
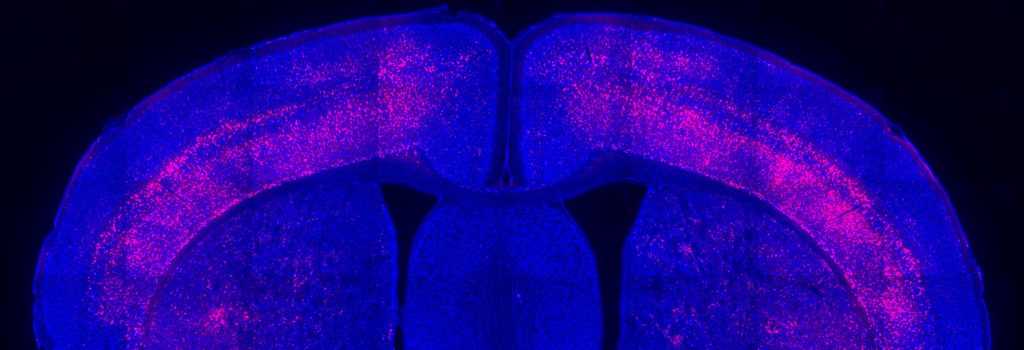
Above: An image from the Choi lab highlights receptors for the cytokine IL-17a in a cross-section of a mouse’s brain.
The study left open questions that, if answered, could enable the development of an immunotherapy for brain disorders. How do immune cells in the gut that produce IL-17a find their way to the brain? How does the molecule then get into the brain, which stringently filters what goes in or out? Once it gets in, how does IL-17a act on brain cells to achieve the symptom improvement? The new project will seek to identify the mechanisms that drive such steps so that they can then be targeted for therapeutic enhancement.
“This is a novel way to think about treating neurological symptoms: using the immune system,” said Choi, Associate Professor in The Picower Institute and MIT’s Department of Brain and Cognitive Sciences, who leads the collaboration. “The question is whether we can use this system to heighten it or dampen it to modulate the brain.”
Four labs, including those of Choi, Huh, and Picower Institute investigators Myriam Heiman, Associate Professor, and Mriganka Sur, Newton Professor of Neuroscience, will collaborate on the project, each bringing very different expertise but also collaborating closely and sharing ideas to tackle the larger problem.
Close and enduring collaboration among newly assembled teams of scientists capable of spanning multiple scales of a complex research question is a hallmark of Simons Center grants, said Sur, who directs the center. This project is the ninth such multi-year “Targeted Project” the center has funded in its 11-year history.
“Progress on major questions in autism requires focused collaboration between researchers using complementary approaches,” notes Sur. “Right now, SCSB is supporting three targeted projects that involve 14 researchers, including cognitive, systems, molecular and computational scientists across building 46 and even outside MIT.”
From gut to brain
A cross-cutting focus of each lab’s research, largely using mouse models, will be studies of the meninges—three layers of connective tissue that surround the brain and anchor it within the head. The meninges may be a critical checkpoint for the transit of immune cells and their IL-17a cargo as it moves from the gut to the brain, Choi said, and although some scientists have hypothesized that cytokines released in the meninges get a free pass into the brain, no one has proven it.
That said, the meninges are just one route that might enable immune system therapies to access the brain, Choi said. Another could lie in finding a way to make the blood-brain barrier more permeable for cytokines, like IL-17a. The team will therefore also look beyond the meninges.
Huh, an immunologist, will work to reveal the molecular logic, or rules, that motivate IL-17a secreting immune cells to migrate from the gut to a place proximate to the brain such as the meninges or otherwise. He’ll seek to identify factors, including the composition of gut bacteria that shape the behavior of immune cells, that might encourage greater migration.
With collaboration from Huh, Choi will lead a project testing ways to compel immune cells that have migrated to release IL-17a to the brain, either systemically or into targeted regions. Choi will also work with Heiman to study the response of neurons to the molecule, for instance by sequencing RNA to see how gene expression changes in the brain cells.
Heiman will also apply her expertise in a technique called TRAP to characterize subtypes of the vasculature and their functions.
Heiman will collaborate with Sur on studies of some of these cells, called astrocytes. Sur’s lab, for instance, will image astrocytes in action as they couple to the brain’s blood vessels and parallel system of glymphatic plumbing both during wakefulness and during sleep when the brain is especially active in flushing cerebrospinal fluid through the glymphatic system. The lab will also track the response of astrocytes to IL-17a in parallel with that of neurons to see how the two cell types interact upon exposure. Finally, Sur will work with both Heiman and Choi to experimentally manipulate astrocyte activity to see how the manipulations affect vascular and glymphatic activity, as well as neuronal response to IL-17a.
Choi notes that if the team is successful in finding ways to encourage therapeutically effective immune system delivery of a cytokine to the brain, their methods might provide a framework for developing immunotherapies for other disorders. The body’s immune responses profoundly affect brain function, Choi notes. We are all familiar, for instance, with how radically our mood, behavior and appetite change when we have a bad cold or the flu, and Covid-19 infection has afflicted many patients with neurological symptoms.
“We want to test the idea of using the immune system to mitigate neurological symptoms,” Choi said. “Although we are focused on autism in this project, I think this idea can translate to any neurological symptoms for any disorder where the immune system turns out to have a role.”