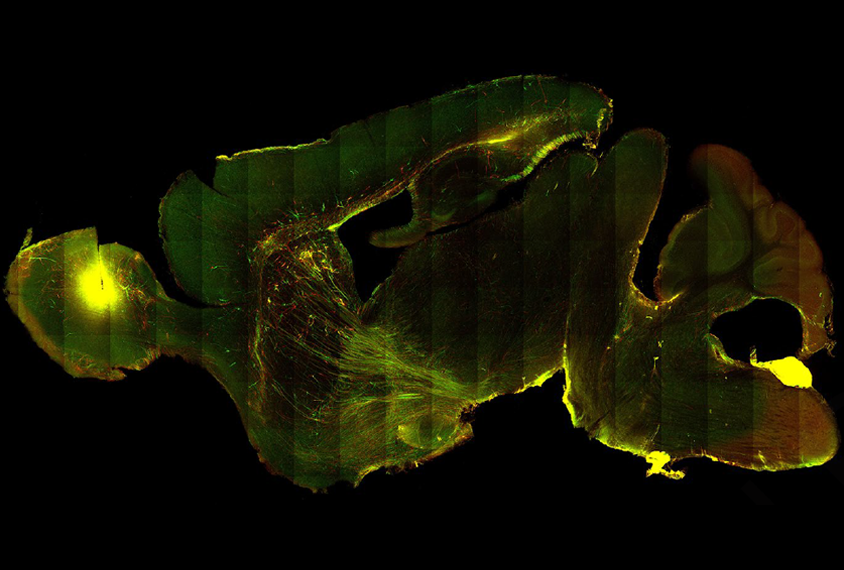
Cell spotting: A brain slice from a chimeric mouse shows cells carrying the fragile X mutation (red) and a typical copy of FMR1 (green), at one month post-injection.
Neurons derived from the cells of a person with fragile X syndrome develop atypically when transplanted into a mouse’s brain, a new study has found. Some of the differences replicate those seen in the brains of people with fragile X syndrome.
Researchers have struggled to create mice that accurately model the condition, which stems from mutations in the FMR1 gene. One of the challenges is that mutations in FMR1 behave differently in mice: Whereas people with fragile X syndrome have an FMR1 gene silenced by 200 or more repeats of a sequence of three amino acids — cytosine, guanine, guanine (CGG) — not even 341 CGG repeats can silence the gene in mice, according to a study published in ENeuro in August.
Efforts to study fragile X neurons in culture have also been unsuccessful. “The neurons pretty much stay immature,” rendering them less useful for identifying and testing potential therapies, says study investigator Marine Krzisch, a postdoctoral researcher in Rudolf Jaenisch’s lab at the Whitehead Institute in Cambridge, Massachusetts.
In the new study, Krzisch and her team combined in vitro and in vivo approaches, enabling immature human-derived cells to develop inside the brains of mice. The chimeric mice were described in Biological Psychiatry in August.
“It’s a very interesting approach,” says Lior Brimberg, assistant professor of neuroimmunology at the Feinstein Institutes for Medical Research in New York, who was not involved in the study. But, she says, there’s “still work to be done.”
Krzisch and her team reprogrammed induced pluripotent stem cells from a person with fragile X into neural progenitor cells — immature cells with the potential to develop into many types of brain cells. They injected the neural progenitor cells into the brains of immune-deficient newborn mice and observed how these cells matured.
Each mouse received four injections — all mixtures of fragile X neuronal progenitor cells and control cells, engineered to have functional FMR1 genes, in the lateral ventricles. Two fragile X cell lines and two control cell lines were tagged with red and green dyes, respectively.
After 15 days, the injected cells appeared in postmortem mouse brains within the corpus callosum, a thick band of cells that connects the left and right hemispheres. After 30 days, the cells had differentiated into neurons and glial cells, a category of support cells that includes astrocytes and microglia, and had traveled to other brain regions, including the hippocampus, cortex, striatum, thalamus and midbrain.
At first, fragile X progenitor cells matured more slowly than control cells that wound up in the same brain areas, an analysis of their gene expression and morphology showed. But after a month, their maturation accelerated. Both cell types reached maturity by six months.
The fragile X neurons showed increased expression of genes thought to be markers of synaptic activity, suggesting that their synapses are hyperexcitable — a finding that matches what researchers have previously observed in fragile X neurons in vitro.
Although the changes in gene expression were expected, another change came as a surprise, Krzisch says: The shape of the fragile X neurons was altered. Typically, the dendrites — small protrusions that extend from a neuron to communicate with surrounding cells — are long and thin in the brains of people with fragile X.
“We basically found the contrary,” Krzisch says, with the fragile X neurons forming shorter dendrites with larger, wider heads.
This finding was “the most intriguing” aspect of the paper, says Hongbing Wang, professor of physiology at Michigan State University in East Lansing, who was not involved in the study. “The data is just opposite to what has been found in animal model and human patients.”
The mouse’s own glial cells surrounded the transplanted cells, which may have contributed to some of the differences, notes Randi Hagerman, medical director of the MIND Institute at the University of California, Davis, who was not involved in the work.
“What happens with the fragile X neuron definitely is related to the status of the astrocytes around the fragile X neuron,” Hagerman says. “And there’s been some studies showing that if you mix normal astrocytes with a fragile X neuron, [the neuron] starts to act normal.”
Krzisch plans to use the new model to probe the influence of microglia on the morphology and function of fragile X neurons. “It’s possible to find phenotypes that were not previously observed using these models,” she says. “We think that’s a good thing.”